
Nội dung bài viết / Table of Contents
This post is also available in: Tiếng Việt (Vietnamese)
Most women experience breast changes at some time. Your age, hormone levels, and medicines you take may cause lumps, bumps, and discharges (fluids that are not breast milk).
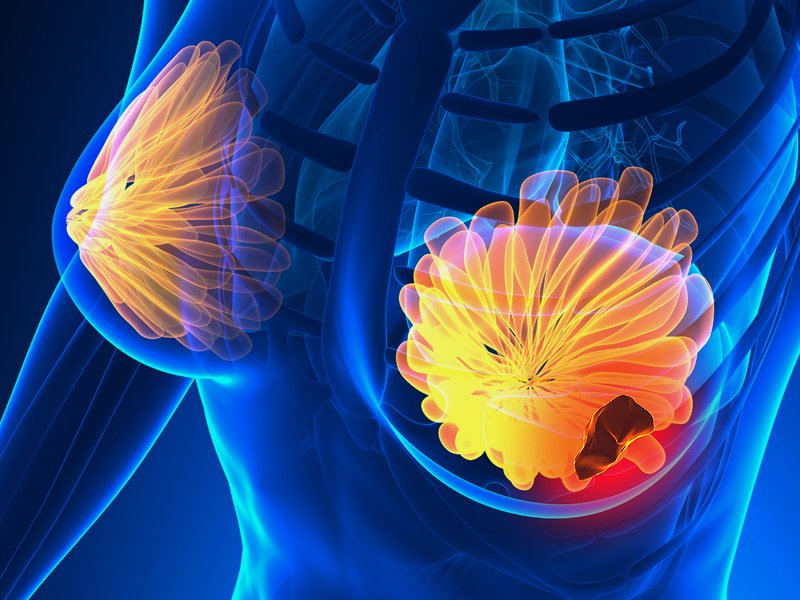
Breast disorders may be noncancerous (benign) or cancerous (malignant). Most are noncancerous and not life threatening. Often, they do not require treatment. In contrast, breast cancer can mean loss of a breast or of life.
Thus, for many women, breast cancer is their worst fear. However, potential problems can be detected early when women regularly examine their breasts themselves, are examined regularly by their doctor, and have mammograms as recommended. Early detection of breast cancer is essential to successful treatment.
Some common breast disorders are:
Breast disorders are common. Please discuss with your doctor for further information.
The common symptoms of breast disorders are:
Breast symptoms do not necessarily mean that a woman has breast cancer or another serious disorder. For example, monthly breast tenderness that is related to hormonal changes before a menstrual period does not indicate a serious disorder.
There may be some symptoms not listed above. If you have any concerns about a symptom, please consult your doctor.
You should contact your doctor if you have any of the following:
The cause of a breast disorder will vary depending on the diagnosis. Some changes simply occur with age or changing hormone levels as the child matures into puberty. Others may be the result of congenital anomalies of the breast, infections, certain medications and genetic or hereditary factors.
Please discuss with your doctor for further information.
The information provided is not a substitute for any medical advice. ALWAYS consult with your doctor for more information.
Breast examination
A breast examination is done. With the woman sitting or lying down, the doctor inspects the breasts for irregularities in shape, a nipple that turns inward (inverted nipple), and lumps.
The doctor also checks for dimpling, thickening, redness, or tightening of the skin over the breast. The nipples are squeezed to check for a discharge. The armpits are checked for enlarged lymph nodes.
The doctor may examine the breast and armpits with the woman in different positions. For example, while sitting, she may be asked to press her palms together in front of the forehead. This position makes the chest muscles contract and makes subtle changes in the breast more noticeable.
The doctor may review the technique for breast self-examination with the woman during the examination. Techniques for the doctor’s examination and self-examination are similar.
Testing
Imaging tests are used to
Mammography involves taking x-rays of both breasts to check for abnormalities. A low dose of radiation is used. Only about 10 to 15% of abnormalities detected by mammography result from cancer. Mammography is more accurate in older women because as women age, the amount of fatty tissue increases, and abnormal tissue is easier to distinguish from fatty tissue than other kinds of breast tissue.
Recommendations for routine screening with mammography vary.
Screening mammography is usually recommended for all women starting at age 50, but some experts recommend starting at age 40 or 45. Mammography is then done every 1 or 2 years. Experts have different recommendations about when to start routine mammography because the benefit of screening is not as clear in women aged 40 to 49. Routine mammography may be stopped at age 75, depending on the woman’s life expectancy and her wish for continued screening.
Mammography may also be done if a woman or doctor finds a lump while examining the breasts or if a woman has breast pain or a discharge from the nipple. It can provide images of any abnormalities (such as a tumor or an abscess) and the tissues around the abnormality. It can also provide images of lymph nodes to check for abnormalities.
Ultrasonography can provide more information about abnormalities detected by mammography. For example, ultrasonography can show whether a lump is solid or is filled with fluid (a cyst). Cysts are rarely cancerous. Ultrasonography can also be used to help doctors place a biopsy needle into the abnormal tissue.
Magnetic resonance imaging (MRI) is done at the same time as mammography to screen women if they have an increased risk of developing breast cancer—for example, if they have a mutation in the gene for breast cancer (the BRCA gene). After breast cancer is diagnosed, MRI is used to identify abnormal lymph nodes and to determine the size and number of tumors. This information can help doctors plan surgery or other treatments.
The treatment options available depend on the type of breast disorder you have. Many types of breast disorders don’t need treatment.
Some growths or masses may be removed surgically. Cysts may be drained using a very fine needle.
Treatment for some common breast conditions:
Fibrocystic breast changes
Most women who have fibrocystic breast disease don’t require invasive treatment. Home treatment is usually sufficient to relieve associated pain and discomfort.
Over-the-counter pain relievers such as ibuprofen (Advil) and acetaminophen (Tylenol) can usually effectively relieve any pain and discomfort. You can also try wearing a well-fitting, supportive bra to reduce breast pain and tenderness.
Some women find that applying warm or cold compresses relieves their symptoms. Try applying a warm cloth or ice wrapped in a cloth to your breasts to see which works best for you.
Fibroadenoma
If you receive a fibroadenoma diagnosis, it doesn’t necessarily have to be removed. Depending on your physical symptoms, family history, and personal concerns, you and your doctor can decide whether to have it removed or not.
Fibroadenomas that don’t grow and are definitely not cancerous can be closely monitored with clinical breast exams and imaging tests, such as mammograms and ultrasounds.
The decision to have a fibroadenoma removed typically depends on the following:
If a fibroadenoma is removed, it’s possible for one or more to grow in its place. Treatment options for children are similar to those followed for adults, but the more conservative route is favored.
Breast cancer
Some treatments remove or destroy the disease within the breast and nearby tissues, such as lymph nodes. These include:
Other treatments destroy or control cancer cells all over the body:
You might get chemotherapy, hormone therapy, or targeted therapy along with surgery or radiation. They can kill any cancer cells that were left behind by other treatments.
Please discuss with your doctor for further information. If you have any questions, please consult with your doctor to better understand the best solution for you.
Sources: