This post is also available in:
Tiếng Việt (Vietnamese)
Definition
What is pancreatitis?
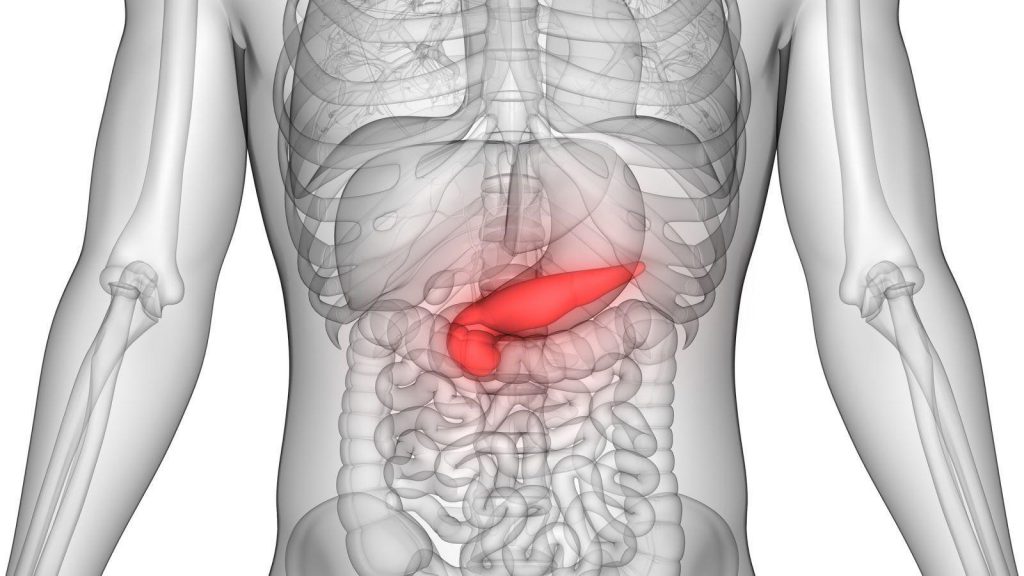
Pancreatitis is pathologic swelling and inflammation of the pancreas. The pancreas is a long, flat gland that sits tucked behind the stomach in the upper abdomen.
It releases digestive enzymes into the small intestine to aid the digestion of food and releases the hormones insulin and glucagon to regulate the way your body processes sugar (glucose). There are two forms of pancreatitis: acute and chronic.
- Acute pancreatitis is a sudden inflammation that lasts for a short time. It may range from mild discomfort to a severe, life-threatening illness. Most people with acute pancreatitis recover completely after getting the right treatment. In severe cases, acute pancreatitis can result in bleeding into the gland, serious tissue damage, infection, and cyst formation. Severe pancreatitis can also harm other vital organs such as the heart, lungs, and kidneys.
- Chronic pancreatitis is long-lasting inflammation of the pancreas. It most often happens after an episode of acute pancreatitis. Heavy alcohol drinking is another big cause. Damage to the pancreas from heavy alcohol use may not cause symptoms for many years, but then the person may suddenly develop severe pancreatitis symptoms.
How common is pancreatitis?
Pancreatitis can affect patients at any age. It can be managed by reducing your risk factors. Please discuss with your doctor for further information.
Symptoms
What are the symptoms of pancreatitis?
Symptoms of acute pancreatitis:
- Upper abdominal pain that radiates into the back, it may be aggravated by eating, especially foods high in fat.
- Swollen and tender abdomen.
- Nausea and vomiting.
- Fever.
- Increased heart rate.
Symptoms of chronic pancreatitis:
The symptoms of chronic pancreatitis are similar to those of acute pancreatitis. Besides, other symptoms are weight loss caused by poor absorption of food. This malabsorption happens because the gland is not releasing enough enzymes to break down food. Also, diabetes may develop if the insulin-producing cells of the pancreas are damaged.
There may be some symptoms not listed above. If you have any concerns about a symptom, please consult your doctor.
When should I see my doctor?
Contact your doctor if you have persistent abdominal pain. Seek immediate medical help if your abdominal pain is so severe that you can’t sit still or find a position that makes you more comfortable.
Causes
What causes pancreatitis?
- Alcoholism;
- Gallstones;
- Abdominal surgery;
- Certain medications;
- Cigarette smoking;
- Cystic fibrosis;
- Endoscopic retrograde cholangiopancreatography (ERCP), when used to treat gallstones;
- Family history of pancreatitis;
- High calcium levels in the blood (hypercalcemia), which may be caused by an overactive parathyroid gland;
- High triglyceride levels in the blood;
- Infection;
- Injury to the abdomen;
- Pancreatic cancer.
Risk factors
What increases my risk for pancreatitis?
There are many risk factors for pancreatitis, such as:
- Heavy alcohol drinking for a long time;
- Certain hereditary conditions, such as cystic fibrosis;
- Gallstones;
- Conditions such as high triglycerides and lupus.
Diagnosis & treatment
The information provided is not a substitute for any medical advice. ALWAYS consult with your doctor for more information.
How is pancreatitis diagnosed?
While asking about a person’s medical history and conducting a thorough physical examination, the doctor will order a blood test to assist in the diagnosis. During acute pancreatitis, the blood contains at least three times the normal amount of amylase and lipase, digestive enzymes formed in the pancreas. Changes may also occur in other body chemicals such as glucose, calcium, magnesium, sodium, potassium, and bicarbonate. After the person’s condition improves, the levels usually return to normal.
Diagnosing acute pancreatitis is often difficult because of the deep location of the pancreas. The doctor will likely order one or more of the following tests:
- Abdominal ultrasound;
- Computerized tomography (CT) scan;
- Endoscopic ultrasound (EUS);
- Magnetic resonance cholangiopancreatography (MRCP).
How is pancreatitis treated?
Treatment for pancreatitis usually requires hospitalization. Once your condition is stabilized in the hospital and inflammation in the pancreas is controlled, doctors can treat the underlying cause of your pancreatitis.
Hospitalization to stabilize pancreatitis:
If you’re experiencing pancreatitis, your doctor may admit you to the hospital for care. Initial treatments to help control the inflammation in your pancreas and make you more comfortable may include:
- You’ll stop eating for a couple of days in the hospital in order to give your pancreas a chance to recover. Once the inflammation in your pancreas is controlled, you may begin drinking clear liquids and eating bland foods. With time, you can go back to your normal diet. If your pancreatitis persists and you still experience pain when eating, your doctor may recommend a feeding tube to help you get nutrition.
- Pain medications. Pancreatitis can cause severe pain. Your health care team will give you medications to help control the pain.
- Intravenous (IV) fluids. As your body devotes energy and fluids to repairing your pancreas, you may become dehydrated. For this reason, you’ll receive extra fluids through a vein in your arm during your hospital stay.
Once your pancreatitis is brought under control, your health care team can treat the underlying cause of your pancreatitis. Treatment will depend on the cause of your pancreatitis, but examples of treatment may include:
- Procedures to remove bile duct obstructions;
- Gallbladder surgery;
- Pancreas surgery;
- Treatment for alcohol dependence.
Chronic pancreatitis may require additional treatments, depending on your situation. Other treatments for chronic pancreatitis may include:
- Pain management;
- Surgery;
- Enzymes to improve digestion;
- Changes to your diet.
See more: Benign neoplasm of thyroid gland
Lifestyle changes & home remedies
What are some lifestyle changes or home remedies that can help me manage pancreatitis?
The following lifestyles and home remedies might help you cope with pancreatitis:
- Stop drinking alcohol. If you’re unable to stop drinking alcohol on your own, ask your doctor for help. Your doctor can refer you to local programs to help you stop drinking.
- Stop smoking. If you smoke, quit. If you don’t smoke, don’t start. If you can’t quit on your own, ask your doctor for help. Medications and counseling can help you stop smoking.
- Choose a low-fat diet. Choose a diet that limits fat and emphasizes fresh fruits and vegetables, whole grains, and lean protein.
- Drink more fluids. Pancreatitis can cause dehydration, so drink more fluids throughout the day. It may help to keep a water bottle or glass of water with you.
If you have any questions, please consult with your doctor to better understand the best solution for you.
Sources: